Heel pain can be a frustrating and limiting condition that affects individuals across various age groups and lifestyles. This discomfort can stem from several underlying issues, and identifying the exact cause is crucial for effective treatment. While heel pain is a frequent complaint, it’s important to understand the diverse factors contributing to it and how to address them appropriately.
Understanding the Root Causes of Heel Pain
Heel pain is not a one-size-fits-all condition. Several distinct factors can lead to pain in the heel, and pinpointing the exact cause is essential for developing a treatment plan. Below, we’ll explore some of the most common causes of heel pain, each with its own set of symptoms and recommended treatments.
1. Plantar Fasciitis: A Leading Cause of Heel Pain
Plantar fasciitis is one of the most common causes of heel pain, particularly in individuals who are on their feet for extended periods. This condition involves inflammation of the plantar fascia, a thick band of tissue that stretches from the heel bone to the toes. Inflammation usually results from overuse or strain, making it a frequent issue among athletes, especially runners, and individuals with jobs that require prolonged standing.
Diagnosis
A podiatrist will start by conducting a thorough physical examination and reviewing your medical history to diagnose plantar fasciitis. They will ask specific questions about the nature of your pain, including when it occurs, its intensity, and any factors that alleviate or exacerbate it. Observation of your gait and additional diagnostic tests, such as X-rays or MRIs, may be necessary to confirm the diagnosis and rule out other conditions.
Treatment
Treatment for plantar fasciitis typically begins with conservative measures such as rest, ice, and stretching exercises designed to alleviate the strain on the plantar fascia. Physical therapy can also play a significant role in recovery, as it helps strengthen the muscles around the heel and improve flexibility. Supportive footwear, including custom orthotics, is often recommended to provide additional support and reduce strain on the affected area. For more severe cases, options such as night splints, PRP therapy, steroid injections, or shock wave therapy may be considered to reduce inflammation and promote healing.
If you are experiencing heel pain that won’t go away, call Foot & Ankle Centers today to schedule an appointment for a full evaluation:
Morris: (815) 942-9050
Yorkville: (630) 553-9300
Risk Factors for Plantar Fasciitis
- Age: Individuals aged 30 to 50 are at higher risk.
- Exercise Routines: High-impact activities such as long-distance running, ballet, or dance aerobics can increase the risk.
- Foot Structure: Flat feet, high arches, or abnormal walking patterns can lead to added stress on the plantar fascia.
- Occupational Hazards: Jobs that require long hours of standing or walking, particularly on hard surfaces, can contribute to the development of plantar fasciitis.
2. Tarsal Tunnel Syndrome: Nerve-Related Heel Pain
Tarsal tunnel syndrome (TTS) is another significant cause of heel pain, stemming from the compression or irritation of the posterior tibial nerve. This large nerve runs from the ankle through the inner side of the heel, and when it becomes inflamed or compressed, it can lead to intense pain and discomfort. TTS can be caused by various factors, including injuries that lead to swelling around the nerve or structural issues such as flat feet.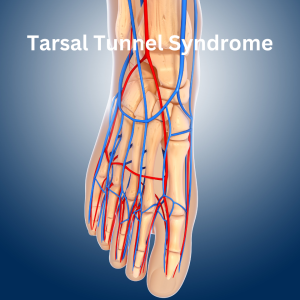
Symptoms
Symptoms of TTS often include numbness, tingling, and pain radiating from the heel to the toes. This pain can sometimes be confused with plantar fasciitis, as it often manifests upon taking the first steps in the morning. However, unlike plantar fasciitis, TTS-related pain may persist even during rest and can evolve into sharp, shooting pain or a burning sensation. Some individuals may also experience weakness in the affected foot.
Diagnosis
Diagnosing TTS requires a detailed assessment by a podiatrist. One common diagnostic tool is the Tinel’s test, which involves tapping on the nerve to see if it produces pain. If TTS is suspected, further confirmation can be obtained through nerve conduction studies or electromyography (EMG) tests performed by a neurologist. These tests measure the speed and strength of electrical signals in the nerve, helping to confirm the diagnosis. MRI scans may also be used to identify any structural issues contributing to the nerve compression.
Treatment
Treatment options for TTS range from non-invasive measures to surgical interventions. Custom orthotics can help alleviate pressure on the nerve, while compression bracing, or supportive socks may reduce swelling. Steroid injections can also be used to decrease inflammation and relieve pain. In cases where conservative treatments do not provide sufficient relief, surgery may be necessary to release the pressure on the nerve and restore normal function.
3. Stress Fractures in the Heel: A Hidden Danger
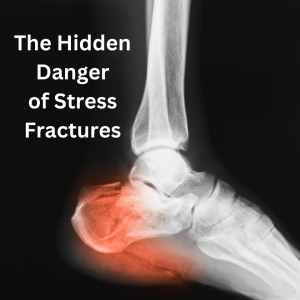 A stress fracture in the heel, specifically in the calcaneus bone, is a less common but serious cause of heel pain. Stress fractures are tiny cracks in the bone that develop over time due to repetitive stress or overuse. Athletes, particularly those involved in high-impact sports like running or basketball, are at increased risk for this type of injury. Left untreated, a stress fracture can lead to significant complications and prolonged pain.
A stress fracture in the heel, specifically in the calcaneus bone, is a less common but serious cause of heel pain. Stress fractures are tiny cracks in the bone that develop over time due to repetitive stress or overuse. Athletes, particularly those involved in high-impact sports like running or basketball, are at increased risk for this type of injury. Left untreated, a stress fracture can lead to significant complications and prolonged pain.
Symptoms
The symptoms of a stress fracture in the heel can be subtle at first, often presenting as a dull ache that worsens with activity and eases with rest. As the condition progresses, the pain may become more severe, accompanied by swelling, bruising, and difficulty walking or standing for long periods. Unlike other types of heel pain, stress fractures tend to cause pain that is localized to a specific area of the heel and may worsen at night or after prolonged periods of inactivity.
Diagnosis
Diagnosing a stress fracture requires a careful evaluation by a podiatrist, who will likely order imaging tests such as X-rays, MRIs, or bone scans to confirm the presence of a fracture.
Treatment
The primary treatment for a stress fracture in the heel is rest. Patients are typically advised to avoid weight-bearing activities to allow the bone to heal. Crutches or a walking boot may be necessary to immobilize the foot and reduce strain on the fracture. Physical therapy can also be beneficial in strengthening the surrounding muscles and preventing future injuries. In severe cases, surgery may be required to repair the fracture and stabilize the bone.
Effective Treatment Approaches for Heel Pain
The treatment for heel pain largely depends on the underlying cause, but several common strategies can be employed to manage symptoms and promote healing. Below, we outline some of the most effective treatment options for various types of heel pain.
1. Custom Orthotics
Custom orthotics are specially designed shoe inserts tailored to the specific needs of your feet. Whether you have flat feet, high arches, or other structural issues, orthotics can provide the necessary support to reduce strain on the plantar fascia and other areas of the foot. These devices are created based on a prescription from your podiatrist and can be an essential component of treatment for conditions like plantar fasciitis and TTS.

2. Night Splints
Night splints are devices worn while sleeping that help stretch the plantar fascia and Achilles tendon, preventing the stiffness and pain that often occurs with the first steps in the morning. By keeping the foot in a dorsiflexed position, night splints can reduce the symptoms of plantar fasciitis and TTS and promote healing during rest.
3. PRP (Platelet Rich Plasma)
Platelet-rich plasma (PRP) therapy is emerging as a promising non-invasive treatment for heel pain, particularly in cases of sub-acute and chronic plantar fasciitis and Achilles tendonitis. By leveraging the body’s natural healing processes, PRP therapy involves injecting a patient’s own platelet-rich plasma into the injured heel tissue, which accelerates tissue repair and reduces pain.
The procedure is safe, quick, and requires no anesthesia or significant recovery time. Clinical studies have shown PRP to be effective in alleviating heel pain, with evidence of tissue repair observed through ultrasound and MRI imaging, offering a potential alternative to surgery.
Schedule Your Heel Pain Consultation Today!
If you’d like to learn more about PRP therapy and whether you are a good candidate for this innovative therapy, call Foot & Ankle Centers today, to schedule a heel pain consultation:
Morris: (815) 942-9050
Yorkville: (630) 553-9300
4. Steroid Injections.
In cases where inflammation is severe, steroid injections may be used to provide rapid relief. These injections are typically administered directly to the affected area, reducing inflammation and pain. While not suitable for all patients, steroid injections can be an effective option for those who do not respond to other treatments.
5. Physical Therapy
Physical therapy plays a crucial role in the treatment of heel pain. Through targeted exercises and stretches, physical therapy can help improve flexibility, strengthen the muscles around the heel, and reduce the risk of future injuries. Physical therapists specializing in foot and ankle conditions can work closely with your podiatrist to develop a customized rehabilitation plan.
At Foot & Ankle Centers we have an excellent Physical Therapy team right next door!
Call (815) 553-2092 to schedule your FREE 15-minute Physical Therapy consultation.
6. Shock Wave Therapy
 Shock wave therapy is a non-invasive treatment that uses high-energy acoustic waves to stimulate healing in the affected tissues. This therapy promotes increased blood flow to the area, which can accelerate the healing process and reduce pain. Shock wave therapy is often used for chronic cases of plantar fasciitis or TTS that do not respond to conventional treatments.
Shock wave therapy is a non-invasive treatment that uses high-energy acoustic waves to stimulate healing in the affected tissues. This therapy promotes increased blood flow to the area, which can accelerate the healing process and reduce pain. Shock wave therapy is often used for chronic cases of plantar fasciitis or TTS that do not respond to conventional treatments.
Taking Control of Your Heel Pain
Heel pain can significantly impact your quality of life, but understanding its causes and the available treatment options can help you regain control. Whether your pain is due to plantar fasciitis, tarsal tunnel syndrome, or a stress fracture, early diagnosis and appropriate treatment are key to recovery. If you’re experiencing persistent heel pain, it’s important to consult with a podiatrist who can accurately diagnose the issue and guide you through the best treatment plan. With the right care and attention, you can alleviate your pain and return to your daily activities with confidence.
If you are experiencing heel pain call Foot & Ankle Centers today to schedule an appointment:
Morris: (815) 942-9050
Yorkville: (630) 553-9300
If you have chronic heel pain Foot & Ankle Centers is here to help. We put your feet first!








